Pneumonia in children is a common disease mostly in developing and underdeveloped countries. There are many etiological causes of pneumonia for example viral, bacterial or fungal. Pneumonia is defined as inflammation of the lung parenchyma associated with recently developed pulmonary radiological shadowing. The world is now familiar with coronavirus which also causes pneumonia in children and adults. Covid pneumonia occurs in both sides of the lung and lobar pneumonia due to bacterial origin usually occurs unilaterally. When a virus or bacteria infects our lung, the immune system makes fight to eradicate the virus. As a result, inflammation damages the lung tissues and makes respiration difficult.
Case Summary
Rihan, a 3 years old boy, the only issue of his non-consanguineous parents, hailing from Chandpur, got admitted with complaints of high grade, intermittent fever for 10 days & non-productive cough for the same duration with breathing difficulty for 3 days. There was no history of runny nose, redness of the eye, evening rise of temperature, alteration of bowel habits, weight loss or contact with a known TB patient. He was treated with syrup cefixime for 7 days.
His birth history was uneventful and developmentally age-appropriate. He is immunized as per the EPI schedule in Bangladesh and had no history of significant past illness. He was on exclusive breast feeding up to 6 months. Then complementary feeding was started. Now he is on the family diet. He belongs to a lower middle-class socio-economic background. His father is a small businessman and his mother is a homemaker. They live in a pacca house and drink tubewell water. Before coming here he was treated with oral cefixime by a local physician for 7 days.
On examination, Siam was ill-looking, febrile, with tachypnoea & tachycardia present, BCG mark present, and anthropometrically well thriving. Respiratory system examination revealed normal chest movement & expansibility on the right side with increased vocal fremitus & vocal resonance, dull percussion note from right 2nd to 4th ICS, and bronchial breath sound with few crackles above that same area. Other systemic examinations revealed normal findings.
Our provisional diagnosis was Right sided consolidation due to pneumonia.
Our differential diagnosis was Right sided consolidation due to Pulmonary tuberculosis or Lung abscess.
To confirm our diagnosis and exclude the differentials we did some investigations.
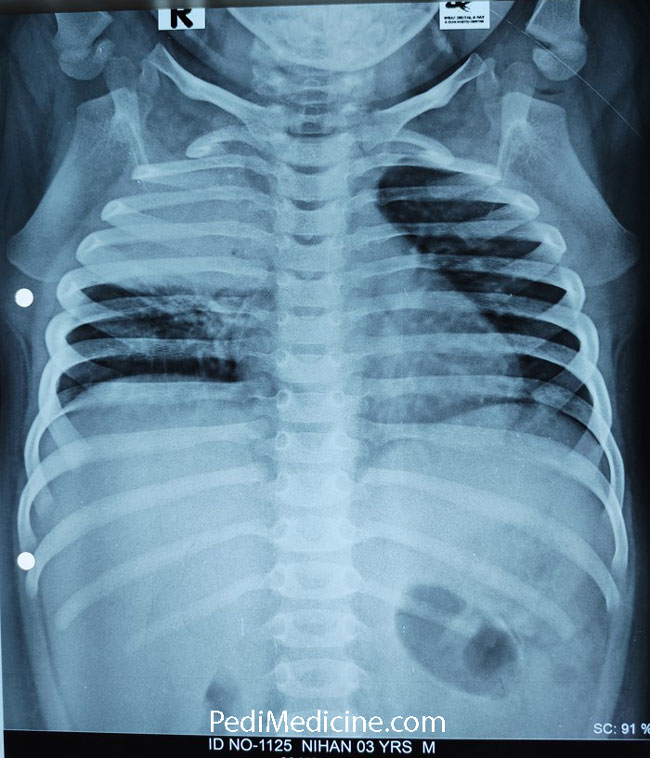
- Chest Xray
- Complete blood count with ESR
- CRP
- Mantoux test
Report of Complete blood count –
- Hb – 12.2 gm/dl.
- ESR – 28 mm in 1st hour
- WBC count: 16,100/cmm
- N – 76%
- L – 17%
- M – 04%
- E – 03%
- Platelet count – 2,38,000/cu mm.
CRP : 17 mg/L
MT: Negative
Chest X-ray: Chest X-ray PA view showing homogenous opacity involving the right upper and middle zone. The trachea is centrally placed and both costophrenic and cardiophrenic angles are clear.
Our final diagnosis was Right-Sided consolidation due to Lobar Pneumonia (Upper lobe)
We treated the patient with IV Inj. Ceftriaxone and he recovered fully.
We managed the patient with
- Counselling regarding the nature and prognosis of the disease.
- Diet: Normal
- Propped up position
- Oxygen inhalation SOS
- Antibiotics: Inj. Ceftriaxone
- Syp. Acetaminophen
- Monitoring of vital signs
- Maintaining temp chart.
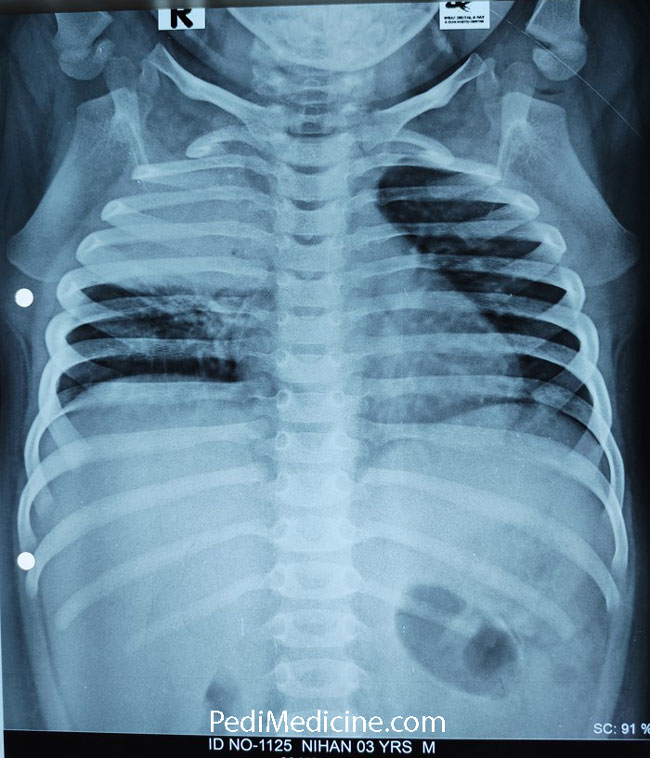
This is the follow-up xray.

Clinical Classification:
1. Community-acquired pneumonia (CAP) i.e. pneumonia acquired from
community/outside hospital
2. Nosocomial i.e. pneumonia acquired from a hospital
3. Pneumonia in special situations e.g.
– aspiration pneumonia,
– pneumonia in an immune-compromised host (opportunistic pneumonia)
Of the different types, CAP is the commonest type.
Risk Factors for developing pneumonia
- Severe malnutrition
- Infectious diseases e.g. measles, pertussis
- Immune deficiency disorders e.g. severe combined immune deficiency
- Congenital lesions e.g. congenital heart (VSD, ASD, PDA) congenital lung diseases
- Younger age e.g. in neonates and infants
- Others e.g. indoor air pollution, over-crowding
Stages of pneumonia :
1. Stage of congestion: Lung parenchyma filled with inflammatory exudate. This allows sound to travel more efficiently, hence bronchial breath sound & increased vocal fremitus develop.
2. Stage of red hepatization: Massive exudation with red cells, neutrophils & fibrin in alveoli.
3. Stage of grey hepatization: Progressive disintegration of RBC with greyish brown discolouration.
4. Stage of resolution: Progressive removal of exudate from alveolar space.
Clinical features
A. Symptoms
- H/O fever followed by cough & respiratory distress
- Fever (moderate to high grade), maybe with chills & rigour
- Cough: may present with intractable cough with productive sputum (sputum amount, colour, if rusty sputum → S. pneumoniae)
- Chest pain (if associated with pleurisy)
- Respiratory distress
- Unable to feed and drink (when respiratory distress is severe)
- In case of mycoplasma: severe headache, muscle pain, body ache, sore throat, breathing difficulty.
- Immunization history
- Associated condition:- Immunocompromised state like HIV, cancer, TB
B. GENERAL PHYSICAL EXAMINATION:
- Appearance: Dyspnoeic, toxic, irritated, Flaring of alae nasi
- Increased body temperature
- Cyanosis, maybe
- Features of respiratory distress:
– Head nodding, present in severe hypoxia
– Grunting may be present in severe cases - SPO₂ normal or may be decreased.
C. CHEST EXAMINATION:
1. Fast breathing:
≥ 60 breaths/min (0-2 months)
≥ 50 breaths/min (2 up to 12 months)
≥ 40 breaths/min (1-5 years)
2. Chest indrawing
3. Tachycardia
Other findings will be variable according to the underlying pathologies.
In pneumonic consolidation: over the affected area→
– Movement restricted on the affected side
– Trachea centrally placed
– Vocal fremitus increased
– Percussion note woody dull
– Breath sound: bronchial
– resonance increased
– coarse crepitation
In Bronchopneumonia, the clinical features are similar to consolidation except that –
The characteristic dullness of lobar consolidation is absent. Breath sound is vesicular instead of bronchial. Crepitation present all over the lung fields
How to Prevent Pneumonia
- Immunization: Against Pneumococcus, Hib, Measles
- Improving nutritional status: By breastfeeding and energy-dense complementary feeding
- Hand washing before handling the young infants
Vaccination for pneumonia in Bangladesh:
In the New EPI schedule, the vaccine available for pneumonia:
1. Pentavalent: against H. influenzae.
3 doses are given at 6th, 10th & 14th weeks.
Was 1st introduced in Bangladesh: January 2009
2. PCV: against pneumococcal bacteria
Dose: 0.5ml, route : I/M
3 doses given at 6th, 10th & 14th weeks
See here for details EPI Vaccine schedule in Bangladesh.
In Bangladesh, PCV was 1st introduced on 21st March 2015 supported by WHO, UNICEF.
Questions:
Is pneumonia contagious?
In general no, but the causative agent is contagious like corona virus as it spreads from person to person.
Walking pneumonia is an informal term for pneumonia that isn’t severe enough to require bed rest or hospitalization. You may feel like you have a cold. The symptoms are generally so mild that you don’t feel you need to stay home from work or school, so you are out walking around. Walking pneumonia spreads through sneezes or coughs. But it spreads slowly. If you get it, you could be contagious (which means you could spread it to other people) for up to 10 days.
Further Study:
Thanks, Everyone.
Leave a Reply